Is My Lower Back or Hip Pain from Sacroiliac Joint Dysfunction?
By William Lian MD
Sacroiliac joint (SIJ) pain has long been an under-recognized and under-diagnosed cause of pain. Lower back pain (LBP) is the most common cause of chronic pain in the United States, with up to 84% of adults experiencing it at some point in their lives.1 Recent studies estimate that the SIJ is the primary pain generator in up to 15-30% of cases of LBP and is a more common in older individuals.2
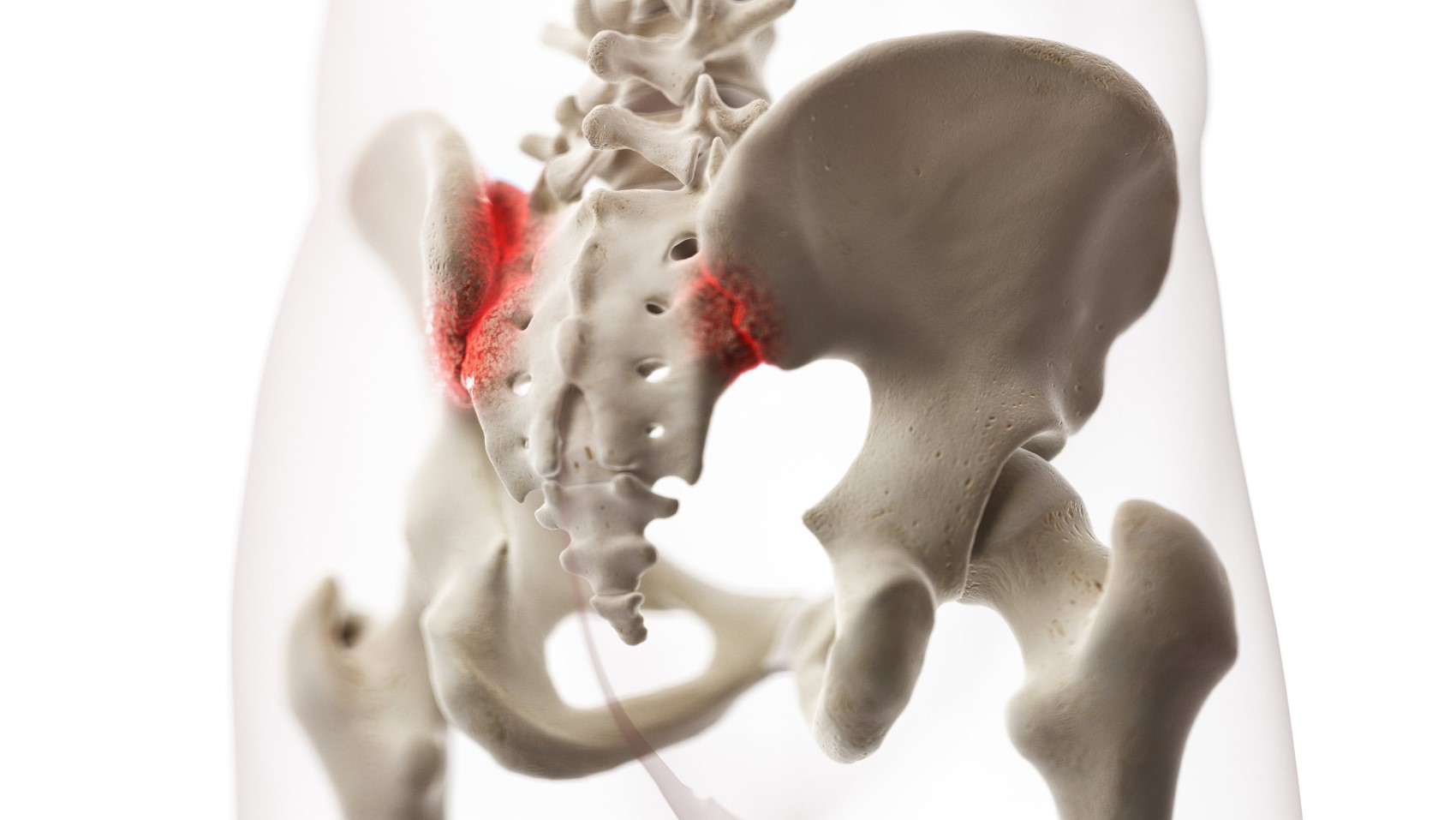
What is the sacroiliac joint?
The SIJ is a diarthrodial joint with complex and variable innervation. The joint connects the sacrum (triangular bone between the lumbar spine and tailbone) and the ilium (top part of the pelvic bone). Ligaments and muscles hold these bones in place and help control the motion of the joint. The range of motion in this joint is small, with studies showing an average rotation of 2.5° and translation of 0.7mm.3 4
How does sacroiliac joint pain occur?
Common causes of SIJ pain are idiopathic (i.e. no clear cause, possible repetitive micro-trauma), degenerative (i.e. arthritis), inflammatory (i.e. rheumatological, autoimmune disorders), and trauma (i.e falls, car accidents). Other less common causes include infection and cancer.5 SIJ pain can also be intra-articular (within the joint) or extra-articular (muscles, tendons, or ligaments outside the joint).6 Pain may also result from a dysfunction, meaning hypermobility (too much motion i.e. pregnancy) or hypomobility (too little motion) of the joint. The SIJ is also a common source of LBP after lumbar fusion to the sacrum due to more force and load transfer to this adjacent non-fused structure.7 Pelvic misalignment associated with leg-length discrepancy, scoliosis, or excessive anterior pelvic tilt (from tight hip flexors and erector spinae muscles combined with weak gluteal and abdominal muscles) can also increase pressure and pain at the SIJ.8
What are the common symptoms of SIJ pain?
Symptoms include pain in the SIJ area which is near the upper medial buttock. Pain is usually worse with transitions including sitting to standing, turning over in bed, and getting in or out of a car. Patients may also have pain walking up stairs, bending and twisting. Symptoms may also include low back stiffness, hip stiffness, and a feeling of being “out of alignment”. Patients with SIJ-mediated pain typically report pain below the L5 region (below top of pelvis), with most localizing their pain to the area around the posterior superior iliac spine (upper medial buttock region).9 One study of chronic low back pain found that older patients without referred thigh pain were more likely to have true SIJ pain (>55%).10 There have also been reports of patients with SIJ pain referring to the posterolateral thigh and even down to the foot along with paresthesias, which mimics lumbar radiculopathy (pinched nerve in the back).11
How do you diagnosis SIJ pain?
At Desert Spine and Sports Physicians, our providers determine if a patient is having SIJ pain based on a thorough history of the patient’s symptoms and a specific series of physical exam tests of the back, pelvis and hips. Imaging with X-Ray or MRI/CT may also be helpful. While imaging may show pathology, in many cases there are no overt findings, and the diagnosis is therefore more of a dysfunction (see above). A fluoroscopically guided intra-articular injection of numbing medication and corticosteroid into the SIJ can help provide diagnostic and therapeutic information.12
How is it treated?
Conservative measures are usually very helpful including an individualized physical therapy program that emphasizes manual therapy to the low back and pelvis and SIJ specific exercises and stretches.13 Anti-inflammatories, muscle relaxants, and other medications as well as ice can be helpful in the acute setting. An SIJ belt may also be helpful in reducing pain and improving stability during walking, though it is best used for short periods to avoid weakening the core muscles.14 An intra-articular injection of steroid can be helpful in reducing inflammation and pain for those who have intra-articular sources of SIJ pain and do not respond to more conservative treatments. Prolotherapy and platelet rich plasma (PRP) are two newer treatment modalities that help target intra and extra-articular sources of pain and recruit the body’s own growth factors for tissue healing and regeneration. Recent studies suggest longer-lasting improvements in SIJ pain and function for patients who received these treatments compared to patients who received steroid injections, with the best outcomes seen in the PRP treatment groups.15 16 17 Radiofrequency ablation or burning of the nerves which innervate the SIJ is another potential treatment option which has been shown to be safe and effective.18 For those who have failed all of the above treatment options, fusion of the SIJ can be considered, though studies show that complication rates tend to be higher with this procedure.19
If you are having pain which may potentially be from your sacroiliac joint, schedule an appointment at Desert Spine and Sports Physicians so that our team of physiatrists can help diagnose and treat your issue. We offer appointments and in-office procedures at all of our Phoenix, Scottsdale, and Mesa locations.
References:
- Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251-258. doi:10.1001/archinternmed.2008.543
- Szadek KM, van der Wurff P, van Tulder MW, Zuurmond WW, Perez RS. Diagnostic validity of criteria for sacroiliac joint pain: a systematic review. J Pain. 2009;10(4):354-368. doi:10.1016/j.jpain.2008.09.014
- Sturesson B, Selvik G, Udén A. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976). 1989;14(2):162-165. doi:10.1097/00007632-198902000-00004
- Wang M, Dumas GA. Mechanical behavior of the female sacroiliac joint and influence of the anterior and posterior sacroiliac ligaments under sagittal loads. Clin Biomech (Bristol, Avon). 1998;13(4-5):293-299. doi:10.1016/s0268-0033(98)00088-6
- Le Huec JC, Tsoupras A, Leglise A, Heraudet P, Celarier G, Sturresson B. The sacro-iliac joint: A potentially painful enigma. Update on the diagnosis and treatment of pain from micro-trauma. Orthop Traumatol Surg Res. 2019;105(1S):S31-S42. doi:10.1016/j.otsr.2018.05.019
- Chuang CW, Hung SK, Pan PT, Kao MC. Diagnosis and interventional pain management options for sacroiliac joint pain. Ci Ji Yi Xue Za Zhi. 2019;31(4):207-210. Published 2019 Sep 16. doi:10.4103/tcmj.tcmj_54_19
- DePalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med. 2011;12(5):732-739. doi:10.1111/j.1526-4637.2011.01098.x
- DonTigny RL. Function and pathomechanics of the sacroiliac joint. A review. Phys Ther. 1985;65(1):35-44. doi:10.1093/ptj/65.1.35
- Dreyfuss P, Dreyer SJ, Cole A, Mayo K. Sacroiliac joint pain. J Am Acad Orthop Surg. 2004;12(4):255-265. doi:10.5435/00124635-200407000-00006
- Laplante BL, Ketchum JM, Saullo TR, DePalma MJ. Multivariable analysis of the relationship between pain referral patterns and the source of chronic low back pain. Pain Physician. 2012;15(2):171-178.
- Hamauchi S, Morimoto D, Isu T, et al. No Shinkei Geka. 2010;38(7):655-661.
- Jung MW, Schellhas K, Johnson B. Use of Diagnostic Injections to Evaluate Sacroiliac Joint Pain. Int J Spine Surg. 2020;14(Suppl 1):30-34. Published 2020 Feb 10. doi:10.14444/6081
- Al-Subahi M, Alayat M, Alshehri MA, et al. The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. J Phys Ther Sci. 2017;29(9):1689-1694. doi:10.1589/jpts.29.1689
- Hammer N, Möbius R, Schleifenbaum S, et al. Pelvic Belt Effects on Health Outcomes and Functional Parameters of Patients with Sacroiliac Joint Pain [published correction appears in PLoS One. 2015;10(10):e0140090]. PLoS One. 2015;10(8):e0136375. Published 2015 Aug 25. doi:10.1371/journal.pone.0136375
- Kim WM, Lee HG, Jeong CW, Kim CM, Yoon MH. A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010;16(12):1285-1290. doi:10.1089/acm.2010.0031
- Saunders, J., 2021. A comparison of ultrasound guided PRP injection and prolotherapy for mechanical dysfunction of the sacroiliac joint – Journal of Prolotherapy. [online] Journal of Prolotherapy. Available at: <https://journalofprolotherapy.com/comparison-ultrasound-guided-prp-injection-prolotherapy-mechanical-dysfunction-sacroiliac-joint/> [Accessed 17 November 2021].
- Burnham T, Sampson J, Speckman RA, Conger A, Cushman DM, McCormick ZL. The Effectiveness of Platelet-Rich Plasma Injection for the Treatment of Suspected Sacroiliac Joint Complex Pain; a Systematic Review. Pain Med. 2020;21(10):2518-2528. doi:10.1093/pm/pnaa170
- Ashman B, Norvell DC, Hermsmeyer JT. Chronic sacroiliac joint pain: fusion versus denervation as treatment options. Evid Based Spine Care J. 2010;1(3):35-44. doi:10.1055/s-0030-1267066
- Lee DW, Patterson DG, Sayed D. Review of Current Evidence for Minimally Invasive Posterior Sacroiliac Joint Fusion. Int J Spine Surg. 2021;15(3):514-524. doi:10.14444/8073
