Osteoporosis and Bone Health
What is osteoporosis?
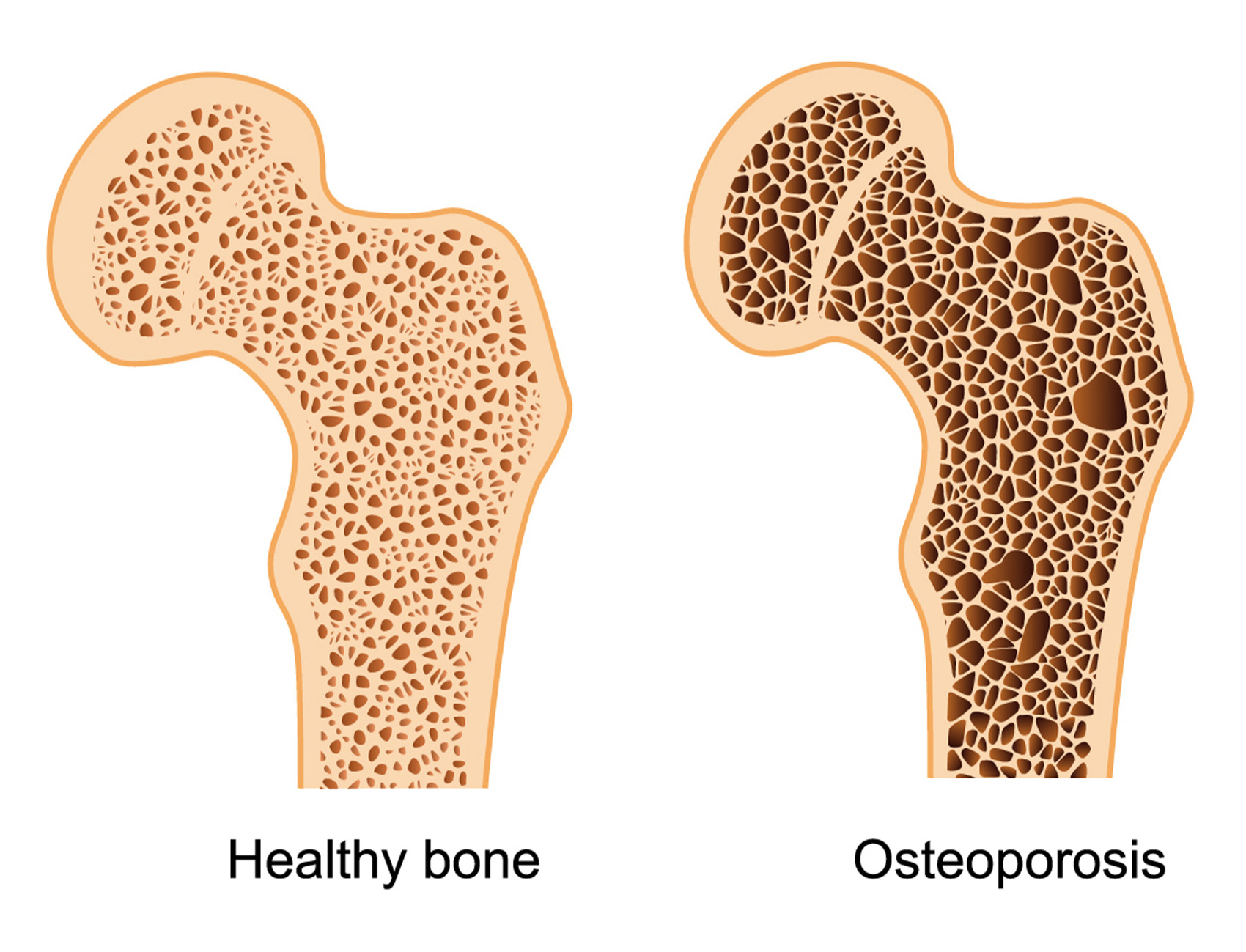
Osteoporosis translates literally as “porous bone” and refers to the loss of the bone mineral density that normally gives our bones structure and support. This typically occurs as we age and is the result of an imbalance between bone formation and resorption. When the bone becomes less dense, it is more susceptible to fractures, especially at the hip and the spine. As a side note, osteoporosis is different from osteoarthritis, which is the wear-and-tear degeneration of a joint.
Are you at risk?
There are both modifiable and non-modifiable risk factors for osteoporosis, including many lifestyle factors. The modifiable risk factors include poor nutrition (especially insufficient calcium and vitamin D intake), inadequate physical activity, cigarette smoking, alcohol consumption, long-term steroid use, and stress. The non-modifiable risk factors include a history of falls, prior fracture, older age, white ethnicity, and female gender.1 Your doctor can estimate your 10-year risk of fracture with a computer-based fracture risk assessment calculator known as FRAX.
What about steroids?
Research has shown that corticosteroid medications (cortisone, prednisone, dexamethasone, and others) can cause an increase in risk of osteoporosis when taken orally or through an IV, particularly if prescribed in a high dose over long periods of time (months or years). However, recent studies have shown that this risk is negligible when the steroids are injected into joints and the epidural space for pain relief procedures.2 This is likely because injected steroids tend to stay in the joint or the epidural space where they are injected, with only a small amount of the medication absorbed into the bloodstream. In fact, in a study of Medicare patients who had received epidural steroid injections, there was a small decrease in the risk of osteoporosis of the spine, though the clinical relevance of the small decrease in risk is not known.3 This may be the result of improved pain and function allowing patients to exercise more regularly. Moreover, improved mobility may limit the fall risk and decrease risk of fracture. What we do know is that long-term use of steroids that are taken up into the bloodstream (oral or IV) increases risk of low bone density, but that the occasional steroid injection is unlikely to contribute significantly to osteoporosis, and could indirectly have the opposite effect.
Getting tested:
A DEXA (Dual-Energy X-ray Absorptiometry) is a special type of X-ray that helps to evaluate the density of your bones. For those at high risk (see risk factors above), a DEXA scan is recommended every 1 to 3 years. A DEXA scan will give you a “T-score” that compares your bone density to a healthy 30-year-old adult. The score classifies your bone density into the normal range (anything above -1.0), osteopenia (between -1.0 and -2.5), and osteoporosis (less than -2.5).
What can you do to prevent or treat low bone density?
It’s no secret that exercise can also help to improve your overall health. In fact, the CDC recommends 150 minutes of moderate-intensity aerobic exercise per week, along with strength training at least twice per week. For more information, see our blog on general exercise recommendations here. In addition to all of the other health benefits of regular exercise, one of the most important ways that you can prevent low bone density is by staying active. According to a recent study, higher total physical activity was associated with overall lower risk of total fractures, including hip fractures.4
In addition, according to the Endocrine Society guidelines, all women undergoing treatment with osteoporosis therapies should consume calcium and vitamin D in their diet or via supplements.5 Vitamin D increases the absorption of calcium and phosphate in the intestine, and numerous studies have shown an increase in bone mineral density while taking the combination of vitamin D and calcium; however, the data on fracture prevention is less clear. The suggested daily dosage for intake is 1200 mg of calcium and 800 international units (IU) of vitamin D, but be sure to ask your doctor before adding these supplements to your daily routine.
What are other treatments for osteoporosis?
For postmenopausal women at high risk of fracture, bisphosphonates are usually the first-line therapy. This is a class of medications that work by inhibiting the breakdown and resorption of bone. These are medications such as alendronate (Fosamax), ibandronate (Boniva), risedronate (Actonel), and zoledronic acid (Reclast). For women at very high risk of fractures, including those with multiple fractures, the Endocrine Society recommends to consider anabolic therapy such as teriparatide (Forteo) or abaloparatide (Tymlos).5 These are synthetic formulations of the natural human parathyroid hormone, and help to stimulate bone formation. In certain cases, hormone replacement therapy could be indicated.
For those who do sustain a fracture in the spine as a result of low bone density, known as a vertebral compression fracture, there are treatment options available. In addition to optimizing the vitamin D and calcium levels and starting medications such as those listed above, procedures like kyphoplasty can help to reduce the pain coming from the fractured vertebral body.
What’s the bottom line?
Osteoporosis can develop in our bones as we age. It is important to understand your individual risk for developing osteoporosis using tools like FRAX and evaluating your bone density using a DEXA scan. With that knowledge, you can take steps to mitigate your risk by performing regular exercise and taking appropriate supplements and medications. If you do develop a compression fracture in the spine, don’t hesitate to contact us to schedule your appointment at Desert Spine and Sports Physicians for an evaluation and treatment recommendations.
References
- Pouresmaeili F, Kamalidehghan B, Kamarehei M, Goh YM. A comprehensive overview on osteoporosis and its risk factors. Ther Clin Risk Manag. 2018. November 6;14:2029–49.
- Kim M, Yang Y, Son H, Huh J, Cheong Y, Kang S, Hwang B. Effect of medications and epidural steroid injections on fractures in postmenopausal women with osteoporosis. Medicine: June 2019. Volume 98; Issue 26:e16080
- Carreon LY, Ong KL, Lau E, Kurtz SM, Glassman SD. Risk of Osteoporotic Fracture After Steroid Injections in Patients With Medicare. American Journal of Orthopedics. September/October 2017:E293–300.
- LaMonte MJ, Wactawski-Wende J, Larson JC, et al. Association of Physical Activity and Fracture Risk Among Postmenopausal Women. JAMA Netw Open. 2019;2(10):e1914084.
- Endocrine Society Clinical Practice Guidelines: Pharmacological Management of Osteoporosis in Postmenopausal Women Guideline Resources. https://www.endocrine.org/clinical-practice-guidelines/osteoporosis-in-postmenopausal-women
